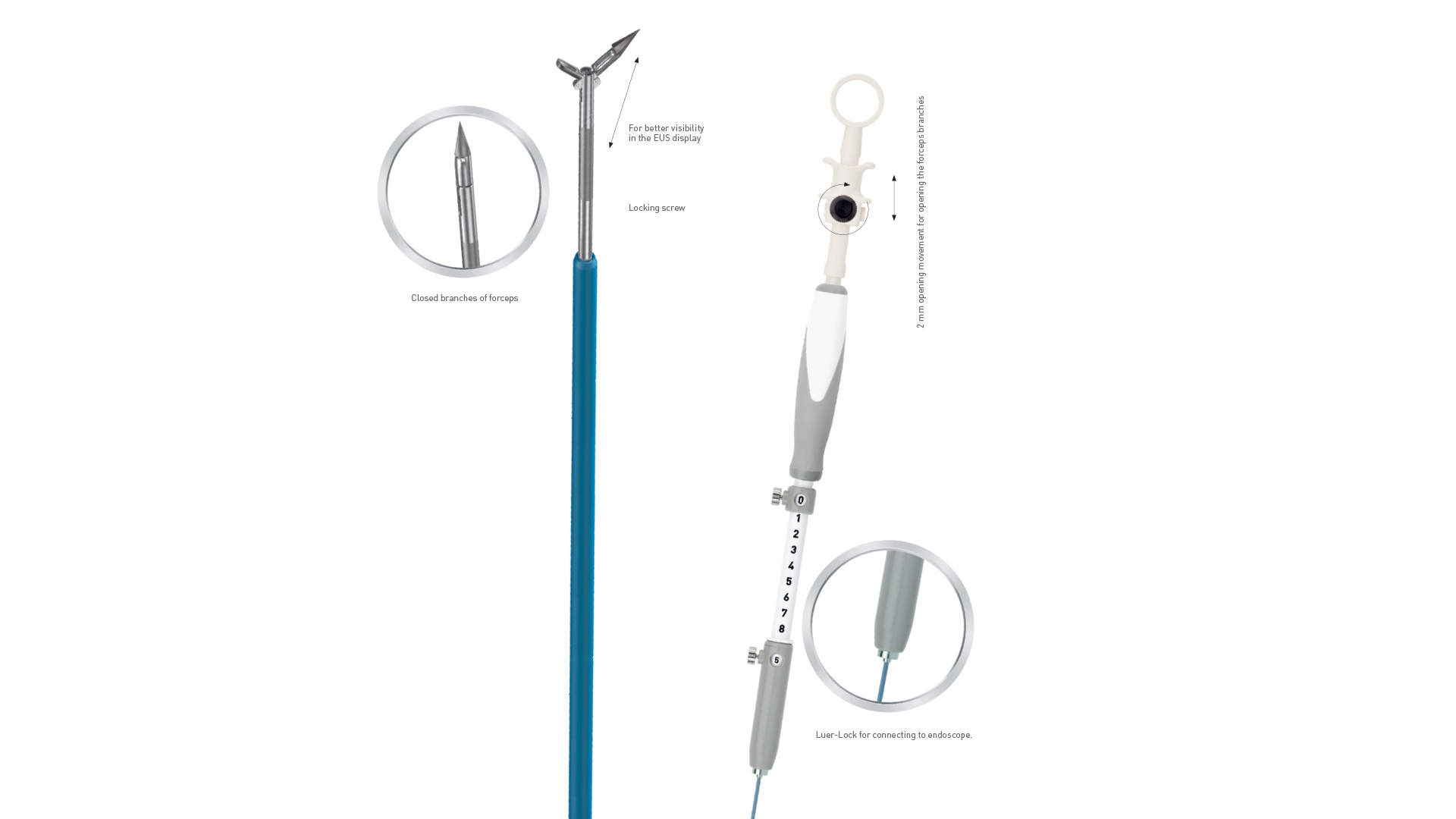
Puncture Biopsy Forceps
The endosonographically controlled harvesting of a tissue sample is usually carried out in the form of fine needle puncture and aspiration. The use of different cut shapes and needle sizes as well as aspiration techniques can improve tissue preservation. However, only single cells or cell groups are often obtained, which only allow the pathologist to cytologically process them. It would be desirable to obtain a histological preparation in order to be able to carry out immunohistochemical examinations, for example.
Material
Pulmonology
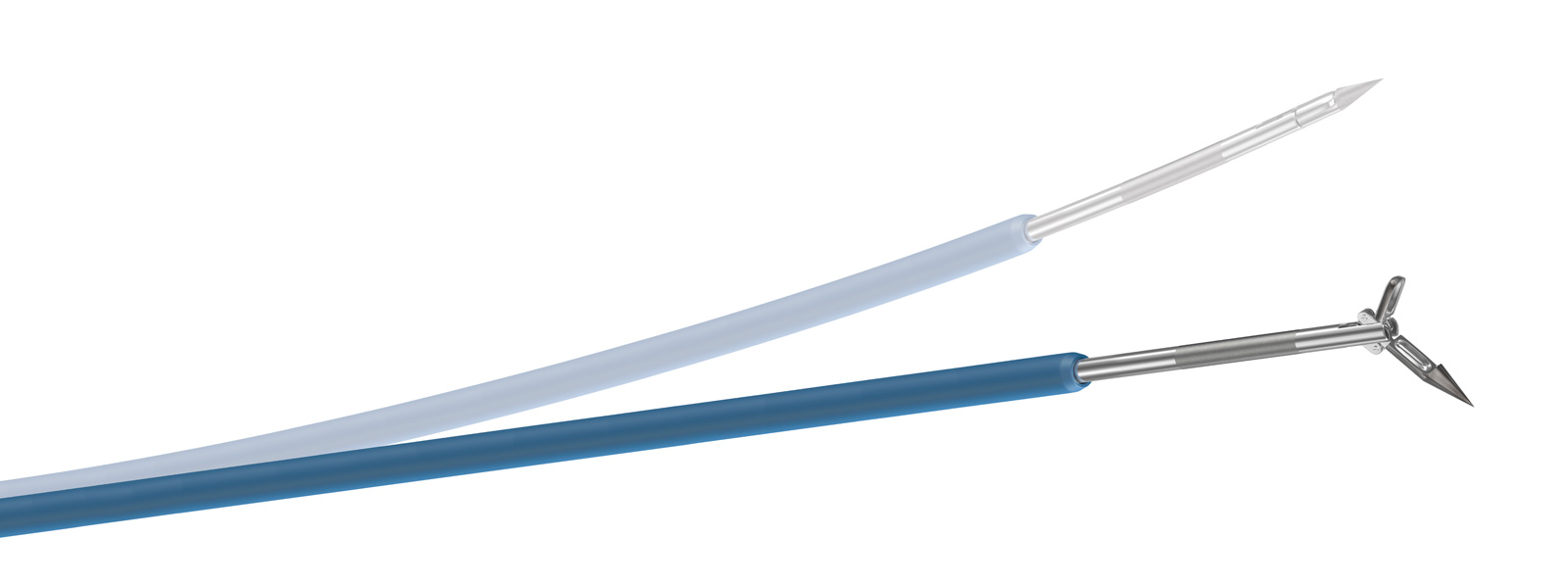
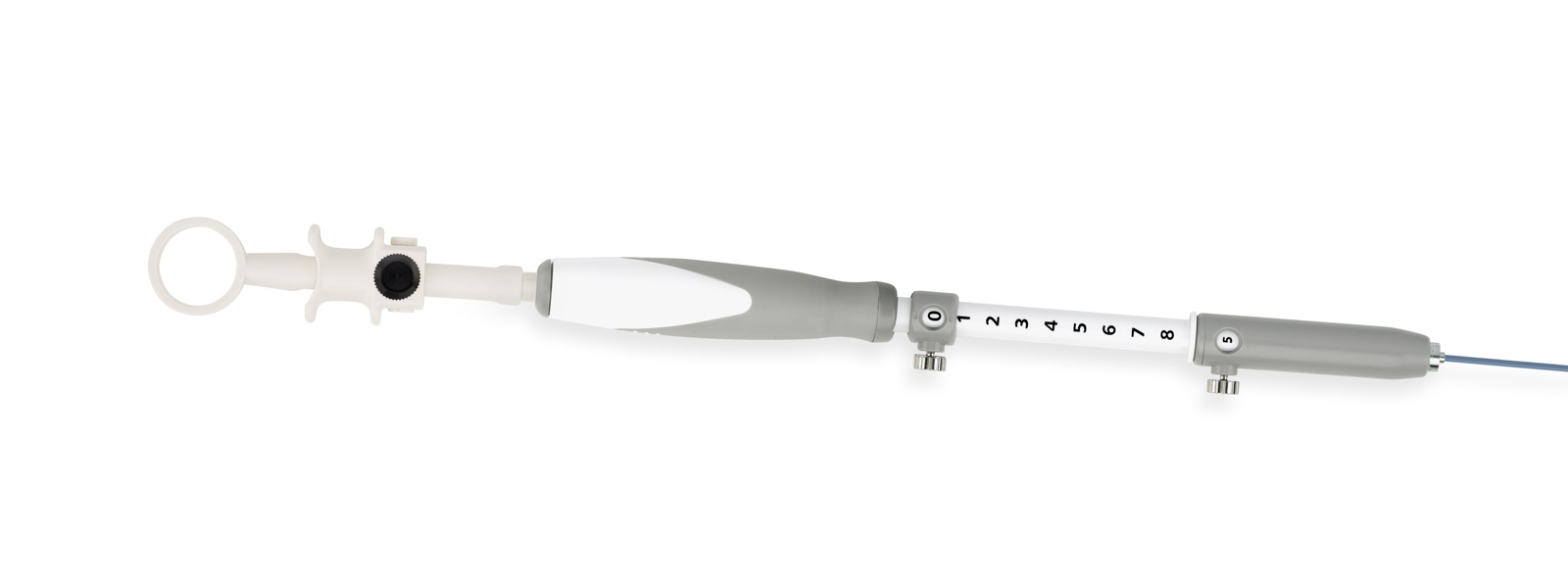
In pulmonology, puncture biopsy forceps are used, which are brought into the lesion in rigid endoscopic technique under radiographic control. These have a needle point at the tip and are equipped with a biopsy forceps, the jaws of which open laterally (see photo). In analogy to this principle, we carried out the first biopsy experiments. However, there was a problem with the correct control of the penetration depth and control of the needle, so that as a further development an EUS puncture needle handle was integrated into this needle by the instrument maker (MTW) (see photo). This ensures safe control. At the same time, the assistant can operate the biopsy forceps.
Result
Advantages
The first application of the new prototype of an EUS puncture biopsy forceps showed a particular advantage in the sampling from cyst walls (pancreatic cyst) and for not very hard lesions. Histology and immunohistochemistry (e. g. GIST in the stomach) were obtained. All in all, the first investigations show promising results with this new method of histology collection under EUS control. Further research series are required, which also include the comparison of the previous method.
First experiences
First experiences with MTW puncture biopsy forceps compared to fine needle aspiration
Case Study
A 36-year-old woman presented with symptoms such as abdominal pain, adiposity and 8 kg weight loss. Computed tomography showed an enlarged pancreas with signs of autoimmune pancreatitis (AIP). On suspicion of autoimmune pancreatitis, an appointment for an endosonography (EUS) with biopsy was scheduled for her.
Endosonography procedure
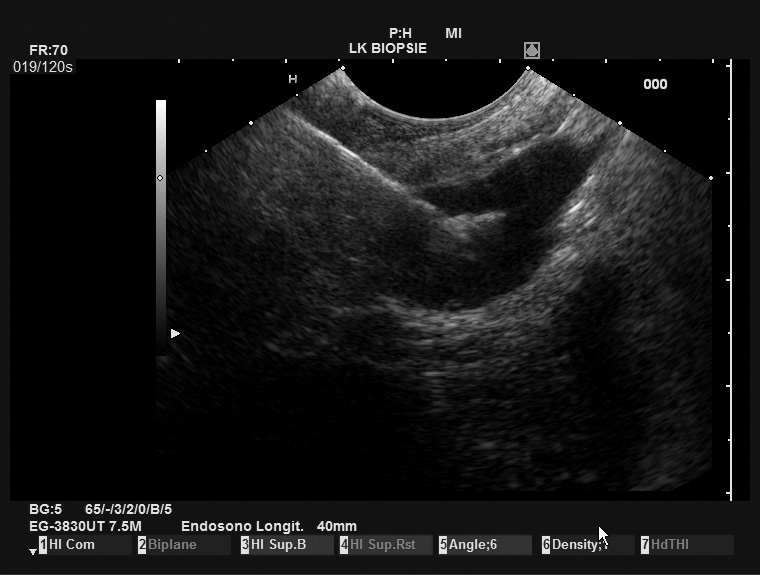
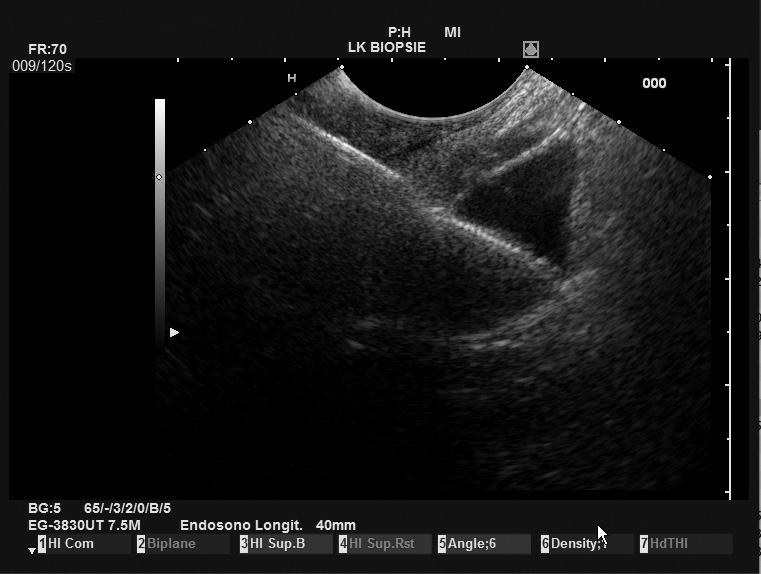
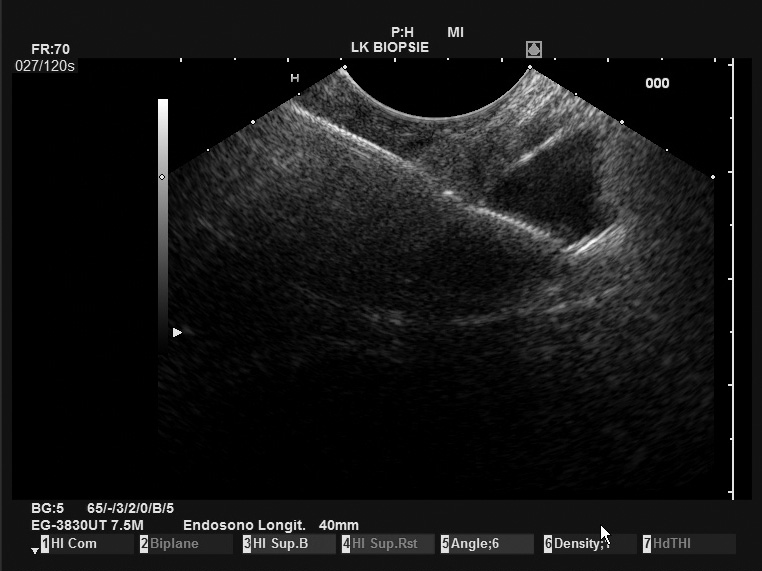
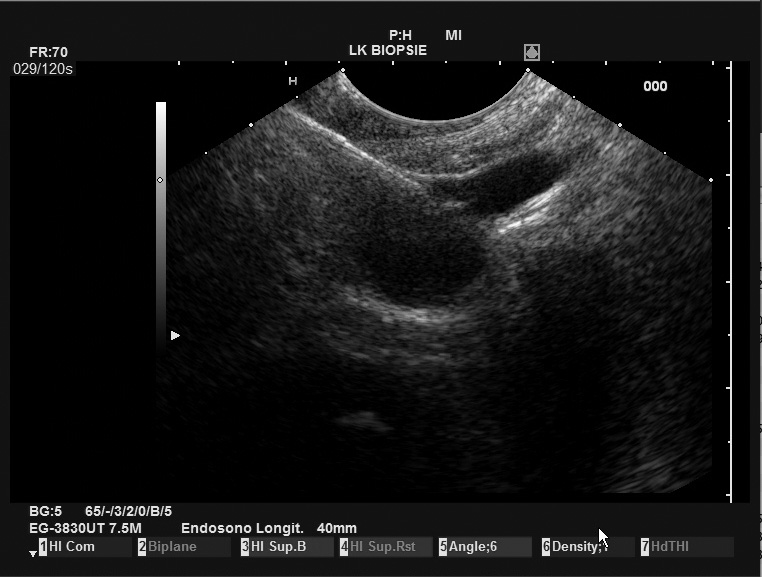
The endosonography procedure was uncomplicated with a simple introduction into the stomach. The pancreatic body and the pancreatic tail were swollen with tangent of the parenchyma and a thin pancreatic duct (1-1.7mm). The pancreatic head was echo-poor and prominent visible. Fine needle aspiration (FNA) was performed twice on the pancreatic body (22G Cook). With the new puncture biopsy forceps (PBF; MTW Endoskopie Manufaktur, Wesel, Germany), 3 biopsies were also taken from the pancreatic body.
Technical experience
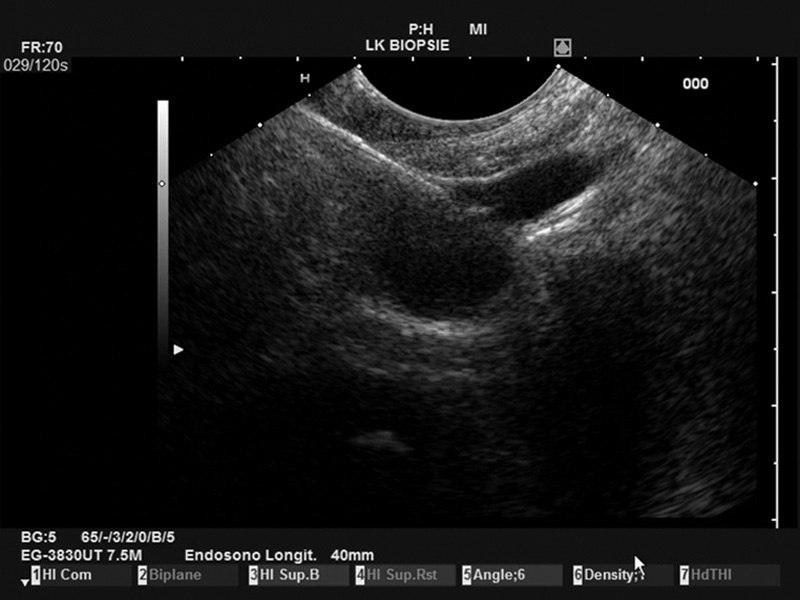
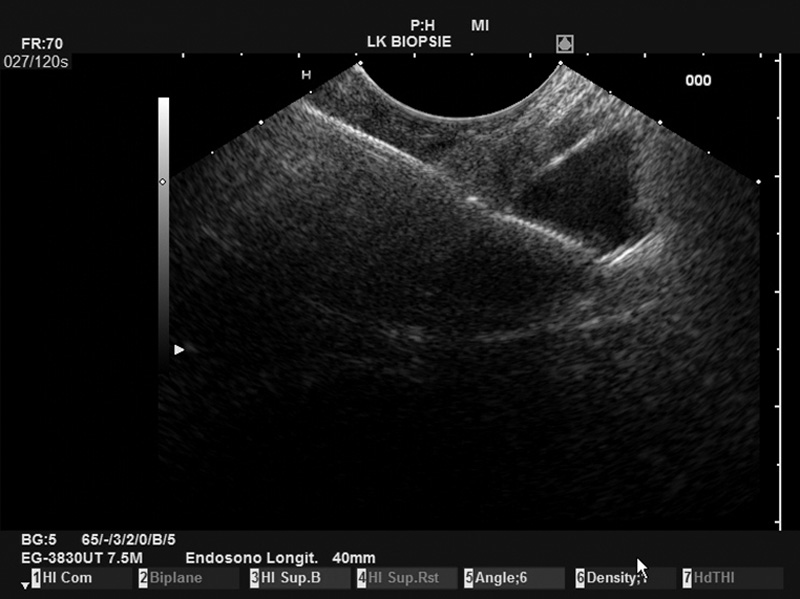
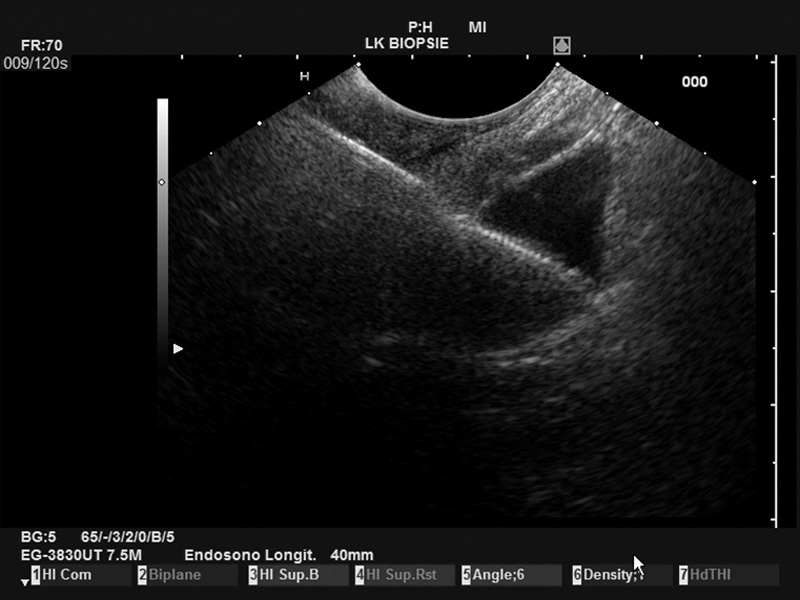
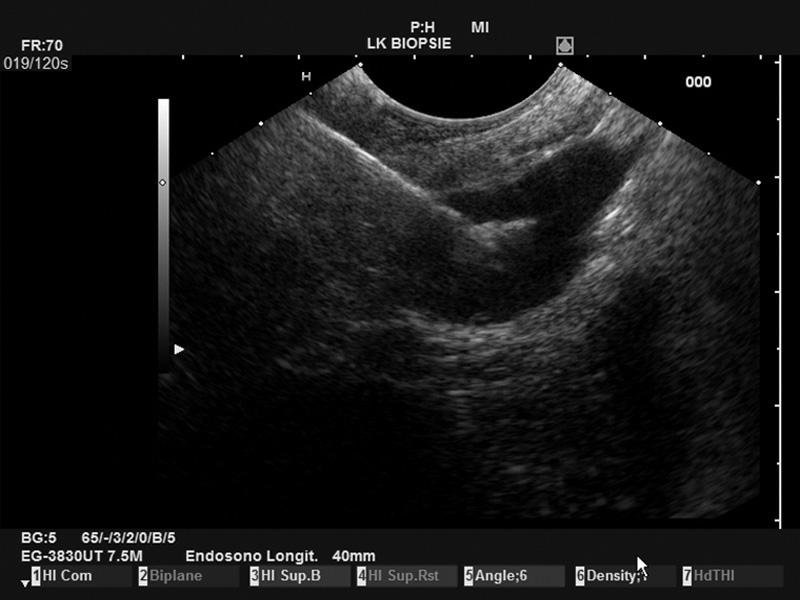
The PBF needle was very sharp, making penetration of the stomach wall and penetration into the pancreatic body easy. In addition, the needle was clearly visible in ultrasound imaging, resulting in good precision. Even the opening of the forceps was clearly visible on the Pentax/Hitachi EUS[Figure 1]. The handle is comfortable to use and the pliers can be easily opened by the assisting nurse. The opening of the forceps is comparable to a gastrobiopsy forceps and is locked in the closed position. This protects the patient from puncture with open forceps with a wide and blunt needle, which can potentially lead to considerable (hazardous) perforation of the puncture channel. The connection of the needle to the ultrasound device was relatively loose, but this does not interfere with the procedure in any way.
Pathological result
The cytological material of the FNA was well assessable and had a high cell density. There were no signs of malignancy or inflammation and no plasma cells were seen. The histological material from the PBF consisted of 4 small tissue components ranging from less than 1mm to 1mm. In the material sections, azina pancreatic tissue was visible without any specific anomalies. It was visible in small amounts of mononuclear inflammatory infiltrate. In order to exclude the diagnosis of autoimmune pancreatitis, additional histology is desirable.
Future research
- Validation of PBF in pancreatic cancer; in the removal of the final diagnosis of pancreatic cancer.
- Assessment of cystic space requirements in the pancreas
- Collection Histopathology of pancreatic cancer for the development of biomarkers and genetic profiling
- Sampling of lymph nodes in lung cancer staging (our pulmonology department is very interested)
- Identification and specification of submucosal gastrointestinal tumors
- Endosonography biopsies of gastrointestinal stromal tumors (GIST) for the determination of C-kit mutations prior to the start of chemotherapy
Possible contraindications
Uncorrected blood coagulation disorders (haemophilia, etc.) Impossibility to make a space requirement clearly visible, a tumor mass or a vessel in the path between the needle and the target site, haemorrhagic diathesis, and risk of tumor scattering PT/INR >1.5, use of anticoagulants and/or heparin.
Conclusion
Our first experience with the first FBP puncture resulted in a histopathology of the pancreas with a very suitable instrument that can be handled very well and accurately. The visibility of the needle is excellent in ultrasound (good opacity), even the small open forceps has been identified with ease on the ultrasound screen. Further research and development is necessary to position their use in the clinical environment.